New Alzheimer’s Study Explores Neuroinflammation and How to Possibly Prevent it
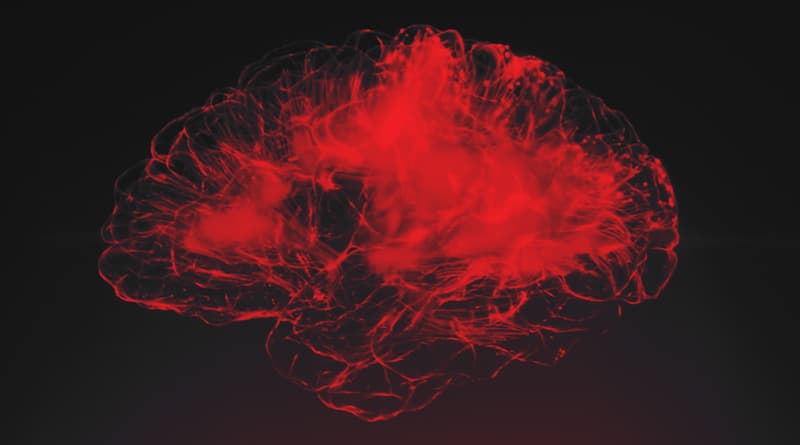
Exploring the Role of Neuroinflammation
Alzheimer’s Disease has a significant impact on every family affected by its grasp, taking a toll both physically and emotionally on everyone involved. Degeneration and deterioration of the brain take away the most fundamental parts of our loved ones, and it can be difficult to watch and experience. However, a new study conducted by researchers at Massachusetts General Hospital(MGH) may shed a new light on the process of brain tissue inflammation and how to prevent it, which in turn can give patients a fighting chance against Alzheimer’s disease.
Plaque on the brain
Today’s scientists have a fair clinical understanding that those with Alzheimer’s have brains that fill with deposits of nerve cells and other proteins that have been damaged. These deposits are referred to as “amyloid plaques”, as well as there being a buildup of entangled clumps of tau proteins. When there is increased activity by a group of enzymes called tau kinases, these enzymes cause the tau protein to clump and become mis-folded, leading to “neurofibrillary tangles”, in turn leading to tau buildup. As Tau builds up in the brain, these formations of entangled proteins can damage brain cells that are vital to both memory and learning. According to neuroscientist and MGH director of the Genetics and Aging Research Unit, Rudolph E. Tanzi, PhD, explains, “if you just have plaques and tangles alone, you probably won’t develop Alzheimer’s disease for a long time, if at all,” rather, the inflammation of brain tissue as a result of these tangles and plaques, or neuroinflammation, is a primary killer of neurons, eventually leading to a decline in cognition.
The Brain’s housekeeper
Prior to Dr. Tanzi’s study, his lab was responsible for the discovery of CD33 back in 2008, the first gene to be associated with neuroinflammation. CD33 is understood to carry the genetic code for receptors on microglia cells, the cells in our brain responsible for clearing away these deposits of amyloid plaques. By 2013, Dr. Tanzi’s team would expand on their findings, concluding that when the CD33 gene is highly expressed, it can negatively influence the activity of microglia, transforming them from the brain’s “housekeeper” to neuron killers, in turn causing neuroinflammation.
The On and Off switch
In the meantime of Dr. Tanzi’s findings, another research team discovered the gene TREM2, which was found to have the polar opposite effect of CD33. While CD33 can activate the neuroinflammative properties of microglia cells, TREM2, vice versa, can actually deactivate the microglia cell’s ability to cause neuroinflammation. Dr. Tanzi strongly believes “The Holy Grail in this field has been to discover how to turn off neuroinflammation in microglia.” So Dr. Tanzi, Ana Griciuc, PhD, and their respective colleagues set off on a genetic expedition; to hopefully find a connection as to how CD33 and TREM2 interact with each other, and to figure out how these interactions have an effect on AD and neuroinflammation when silenced individually or at the same time.
A connection between CD33 and TREM2
So Dr. Tanzi’s research team bred a population of laboratory mice, genetically designed to have brain changes/behavior similar to those with Alzheimer’s disease. The research team began to observe a strain of these AD mice that had their CD33 genes switched off, followed by their ability to learn and memorize through rigorous activities, such as navigating a maze. Surprisingly, these mice with deactivated CD33 had reduced levels of amyloid plaque, and increased their level of performance in learning and memory. However, if both CD33 and TREM2 deactivated simultaneously, or if TREM2 was deactivated alone, these benefits were not present and did not positively impact learning and memory in AD mice. “That tells us that TREM2 is working downstream of CD33 to control neuroinflammation,” according to Dr. Tanzi. Through the sequencing of microglia RNA, this theory was reinforced, indicating that both CD33 and TREM2 work in tandem to regulate neuroinflammation, by increasing and decreasing the level of activity in the immune cell IL-1 beta and and the cell receptor IL-1RN.
Dr. Tanzi expressed that, “We are increasingly realizing that to help Alzheimer’s patients, it is most critical to stop the massive brain nerve cell death that is caused by neuroinflammation,” and would detail that, “We now see that the CD33 and TREM2 genes are the best drug targets for achieving this goal.” We’re slowly but surely beginning to understand the workings of Alzheimer’s, and every finding will advance us toward improved solutions for our loved ones that live with this debilitating disease.
What can I do to help my loved one?
So what can you do for your loved one with Alzheimer’s to help them? Take the time and patience to educate yourself and the family on what your loved one is going through, both physically and mentally. Converse with them, expose them to the outdoors to prevent depression, and give opportunities for activities to exercise both physically and cognitively. Make family time, and listen to their needs and concerns. Remind them how much they are loved and supported, and they have someone by their side, no matter what.
Sources: Alz.org, Science Daily
Derek Dunston has worked in children’s entertainment for several years, through balloon art, magic, music, and educational games. He is working towards his B.A.S. in Secondary Mathematics grades 6-12 and has served Broward County Public Schools as a substitute teacher for three years. He plans to dedicate his life to child honoring and promoting inclusive/multicultural practices to benefit future communities in the fields of education and children’s entertainment.